SHE WAS PROBABLY A TOMGIRL who knew how to whistle with her fingers. Today, she is a mother with an infectious laugh, who, at the moment, is tearing through a room, gently ignoring her son while telling him he is acting “weird,” as she lifts her little girl to the sky.
We caught Lauren in one of her rare free moments. I hadn’t planned to interview her. Once she agreed, I estimated that we had about 15 minutes. It turned out to be less. I understood that her work is in palliative care, and wondered, among other things, how she managed to compartmentalize the challenges of that job and her home life, if that’s what she did.
What I heard is that her job is one part of one piece, and that she’s all there wherever…for whomever. She doesn’t believe in God, yet her empathy for patients is palpable. (She unsuccessfully fought back tears when recalling someone who had just passed.)
Towards the end of our conversation, the kids expressed an urgent interest in a place not where they were, and she was off.
“I hope that [meaning our talk] was okay?” she asked while leaving.
“It was totally okay!” I shouted.
I don’t think she heard me.
What brought you to Santa Fe?
My parents lived here, and my husband, Mac, was finishing up a residency in Washington State. He was fluent in Spanish and wanted to work at an FQHC [Federally Qualified Health Center]. So, during his third year of residency, he came down here for three months, worked at La Familia [La Familia Medical Center], loved it, and wanted to move down here. That was six years ago.
The plan was to stay for three years; I was going to finish my masters and then we were going to head back to New York.
Famous last words. And your Masters is in nursing?
Yes, I’m a Palliative Care Nurse Practitioner for Christus St. Vincent. Palliative care focuses on quality of life for people with terminal illnesses. It’s hospice, but hospice is not palliative care. We focus on symptoms, on goals of care, on family support, and what a patient wants at the end of life.
It must be difficult.
It’s actually a quite freeing approach, because our medical system can be suffocating with treatments and “the next step.” There’s far too little discussion of what quality of life is, especially for really sick people, so I can free my patients from that hamster wheel. I have no reason to try to save someone’s life, or be God, which is often the case in Western medicine.
Still…the end of the work process is death, right?
Yes, but that’s the end result of many professions in healthcare, because death comes to us all.
I mean, you’re very funny. Your wit and way of looking at the world is written into your process. How do you splice that with a situation in which people are likely very upset?
I do use humor, definitely, because it can help them understand that this might not be as serious as they think it is…because death is part of life, and I try to make it not such a big deal that it is maybe closer than they had hoped.
I’m sure you have encountered different attitudes. One of them has to be denial.
Absolutely, that can be a stage. I’ll see people for a week or two weeks initially, and we talk about it, and some people aren’t ready to acknowledge it, and may die within the denial stage. Some…they get past it and have more freedom, in a way.
WANT TO READ MORE? SUBSCRIBE TO SANTA FE MAGAZINE HERE!
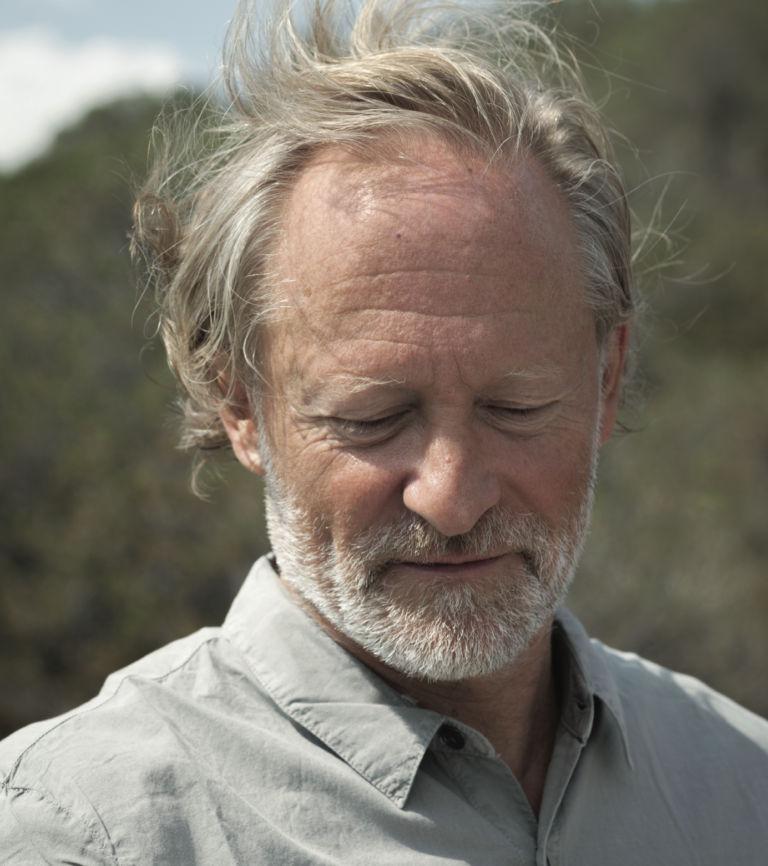
Photo Mary Moon